
Data Illustrates Need To Protect State Investments Aimed At Improving Maternal And Child Health Outcomes
Digital Briefs
March 28, 2019
Citizens’ Committee for Children of New York today released a data infographic that illustrates the critical importance of New York State’s investments in child and maternal health and calls for immediate action in Albany’s budget negotiations to reject proposals that would jeopardize the health and well-being of vulnerable New Yorkers.
While New York City has experienced important progress in reducing the infant mortality rate citywide, disparities persist across racial/ethnic groups and communities.
The data in our infographic make clear the importance of legislation to establish a statewide Maternal Mortality Review Board, which has passed the Senate and Assembly and is awaiting the Governor’s signature.
However, the data also make urgently apparent the need to strengthen New York City’s community health infrastructure — an infrastructure now threatened by the Governor’s proposal to cut State reimbursement to New York City for the General Public Health Work (GPHW) program by $59 million.
Below is an overview of key areas where New York still has work to do to improve infant and maternal health outcomes.
Infant Mortality Is A Citywide Issue, But It Disproportionately Impacts Communities Of Color
The city’s historically low Infant Mortality Rate (IMR) reflects important investments to improve infant and maternal health outcomes. However, stark racial/ethnic disparities in IMR persist. Compared to non-Hispanic white infants, the mortality rate is three times higher for black infants and one and a half times higher for Hispanic infants.
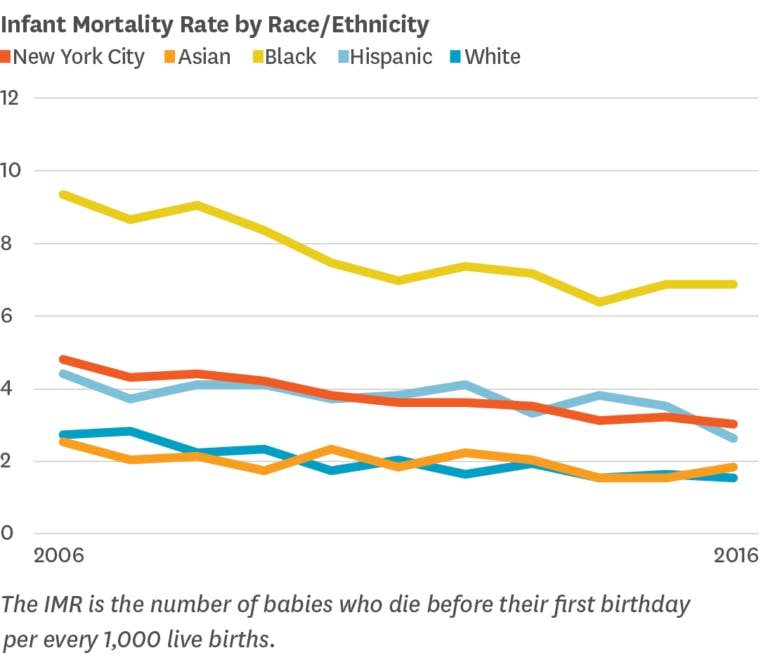
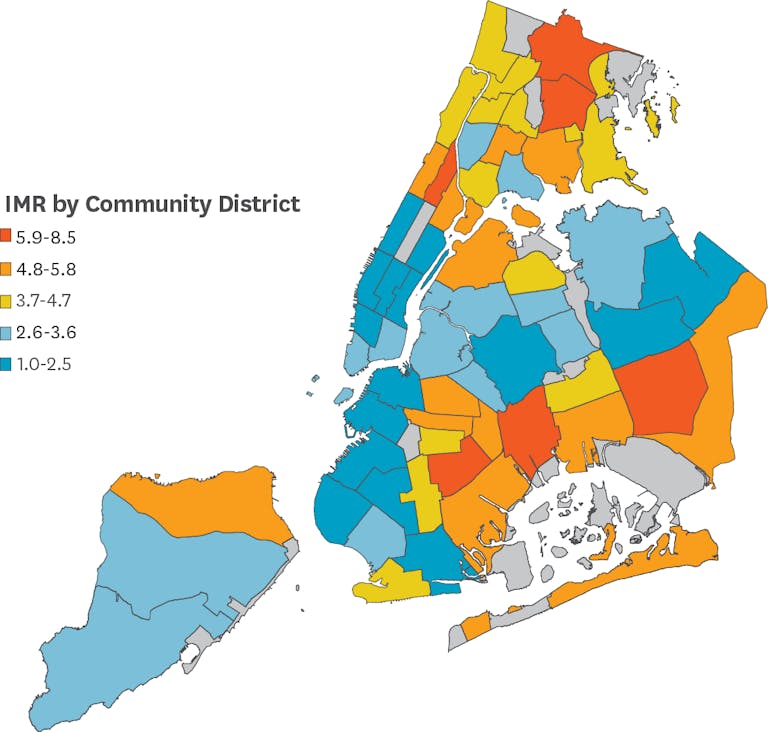
IMR rates also vary widely by neighborhood, reflecting underlying social and economic disparities. In areas with very high poverty, the IMR rate is nearly two times higher than in areas with low poverty.
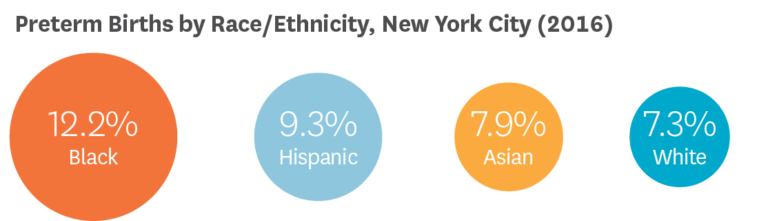
For every white baby born too soon, there are two Black babies born preterm. Racial disparities in birth outcomes persist even when adjusting for factors like socioeconomic status and prenatal care.
Preterm Birth And Low Birthweight Are Leading Causes Of Infant Mortality
Even though they are less than five miles apart, Park Slope has the lowest percentage of babies born at low birthweight in the city, while Brownsville has the highest. Geographic disparities reflect a range of structural, historical and systematic factors impacting community resources and outcomes, including racial segregation, concentrated poverty, and availability of quality care.
Black Non-Hispanic Women Face A Severe Maternal Morbidity Rate Three Times That Of White Non-Hispanic Women
For every maternal death, there are an estimated 100 instances of life- threatening complications from delivery. Racial disparities in SMM persist even when accounting for factors like education and Body Mass Index, reflecting the stressors of individual and structural racism.
As with SMM, Racial disparities in Maternal Mortality remain stark in New York City. Black women account for only 23% of births in NYC, but 57% of pregnancy-related deaths. Asian/Pacific Islander and Hispanic women also faced heightened risks.
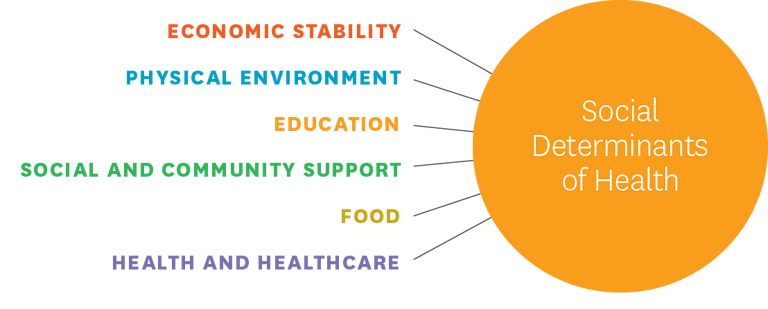
Improving Maternal And Child Health Outcomes Requires Tackling Community And Social/Economic Inequities
To improve infant and maternal health outcomes, New York must ensure that every woman has continuous, high-quality, respectful healthcare before, during, and after pregnancy, as well as the resources necessary to support herself and her family. Increasing access to doulas, midwives, and home visiting programs, promoting group prenatal care, and strengthening connections to community-based organizations are just some of the ways to improve maternal and child health.

Improving child and maternal health requires a multifactorial approach, including strategies to improve hospital protocols for obstetric patients, increasing use of progesterone for high-risk moms, and helping women prevent and manage chronic conditions. It also requires investments in interventions that promote safe sleep practices, support breastfeeding moms, and assist with smoking cessation.
Combatting disparities in health outcomes also requires addressing Social Determinants of Health, or the conditions in which people are born and live that impact their overall health. Issues like structural racism, income inequality, housing instability, and disparate treatment in health- care settings all contribute to chronic stress and disparities in health outcomes.
Reducing Barriers To Safety Net Services Is Crucial For Improving Maternal And Child Health
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) provides free healthy food and resources to women and children, including breastfeeding support, nutrition counseling, and referrals. However, some eligible families don’t enroll due to stigma, lack of information, and other access barriers. Recent federal policy proposals targeting immigrant communities are making many New Yorkers afraid to access services like WIC.


